| Outbreak: Reusable Shopping Bag |
|---|
| Product: Reusable Shopping Bag |
| Investigation Start Date: 10/13/2010 |
| Location: Single County |
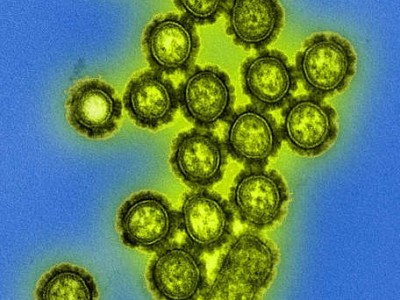
| Etiology: Norovirus |
| Earliest known case onset date: 10/10/2010 |
| Latest case onset date: 10/12/2010 |
| Confirmed / Presumptive Case Counts: 7 / 5 |
| Positive Samples: 1 |
| Outbreak Summary: |
|---|
| Health officials made a rare discovery with this outbreak by identifying a reusable shopping bag as the vehicle for norovirus investigation. The reusable shopping bag was stored in a bathroom used by the index case during her illness onset. The bag contained cookies, chips and other food items that were eaten by tournament attendees who subsequently became ill. Documents
Media Coverage |
| Details: |
|---|
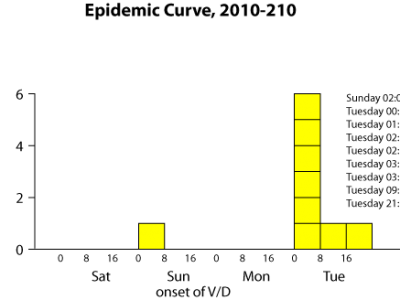
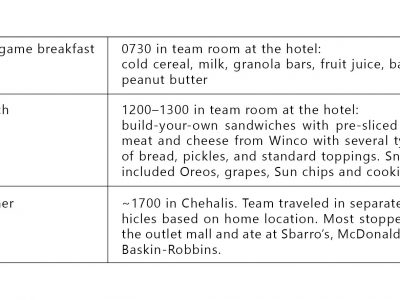
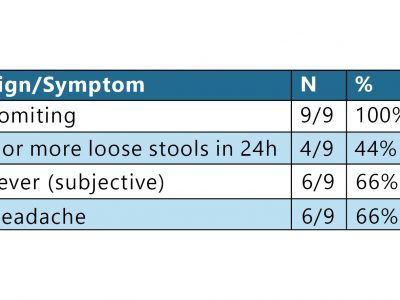
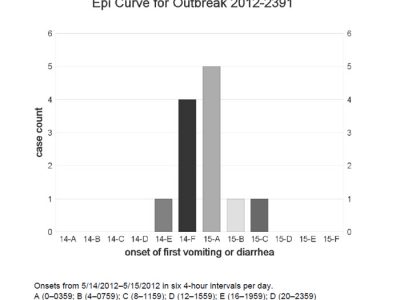
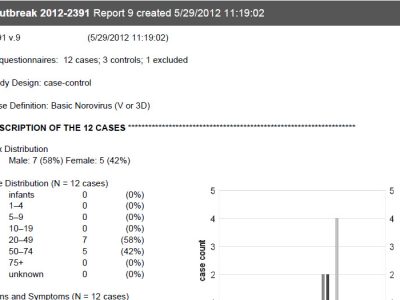
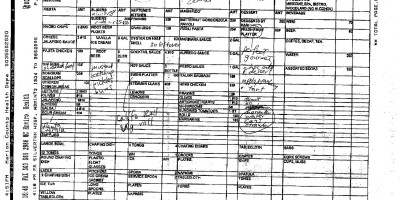
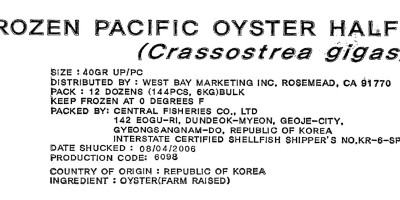
| Introduction On October 13, 2010, the Washington County (Oregon) Health Department was notified by epidemiologists from the Washington State Department of Health (WSDH) and Public Health—Seattle & King County (PHSKC) about an outbreak of gastroenteritis affecting members of an Oregon soccer team. The soccer team had arrived in Redmond, Washington, on Friday, October 8; its members ate in restaurants around town and also consumed homemade items that they had brought with them. Early the morning of Sunday, October 10, one girl became ill with vomiting and diarrhea and was driven home that day by one of the parent chaperones. A fellow team member, unaware of her teammate’s illness, went into the vacated room and found a reusable plastic grocery bag, containing lunch items, which was stored on the floor of the bathroom. On Tuesday, October 12, other team members and chaperones became ill, and one of the parents notified PHSKC. Methods While epidemiologists of WSHD and PHSKC canvassed tournament organizers about any similar reports from other teams, Oregon epidemiologists obtained a team roster and chaperone list. Twenty-one interviews were conducted over the phone or in person at a team practice on Thursday, October 14. One healthy person refused the interview. One ill person was excluded from analysis due to direct exposure to the index case and her vomiting. Cases were defined as group members who developed vomiting or diarrhea (≥3 loose stools within a 24-hour period) during October 9–13. The follow-up questionnaire specifically targeted meals and all reported food exposures on Friday, Saturday and Sunday, October 9–11. Stool specimens were solicited from persons who had been ill. A reusable grocery bag was tested for norovirus by swabbing small patches of the bag’s surface. Swabs of the surface of the reusable grocery bag were tested for norovirus by real-time, quantitative reverse-transcription polymerase chain reaction (RT-qPCR). Results Nine primary and five secondary cases were identified. The noroviral etiology and tight clustering of the Tuesday, October 12, case onsets suggested a common exposure on Sunday afternoon—most likely lunch or something at stopover on the drive home. In the initial cohort analysis, only eating cookies from an unopened package on Sunday at lunch was significantly associated with illness, with 3 of 7 cases consuming and none of 12 healthy cohort members exposed (risk difference [RD] 0.750; 95% CI 0.24–0.91; P = .01). After cases were re-interviewed with the focused questionnaire, investigators learned that the packaged cookies, packaged chips, and fresh grapes had been stored together in a reusable plastic shopping bag with an open top. Further, said shopping bag had been stored in the hotel bathroom where Case 1 had been vomiting throughout the night. Investigators then created a composite variable to include all three items in the bag. All 7 cases but only 4 of 12 healthy cohort members had consumed at least one of the 3 items in the bag (RD 0.636; 95% CI, 0.32–0.87; P < .01; see the published journal article for further analysis detail). Norovirus genotype GII.2 sequence was detected by RT-qPCR in all 3 stool specimens collected from cases and in swabs of the reusable plastic shopping bag. Lessons learned & historical significance This outbreak highlights the risk of acquiring noroviral gastroenteritis from a fomes, the surface of which can be contaminated when left in an enclosed environment with someone who is vomiting. Any surface—not just a visibly soiled one—exposed to an ill person should be fully disinfected. Food and drink should not be stored in toileting areas; anything stored in areas where someone has vomited should never be consumed. |