| Outbreak: Lian How White Pepper | |
|---|---|
| Product: White Pepper | Investigation Start Date: 03/02/2009 |
| Location: Multi-state outbreak–OR, CA, NV, WA | Etiology: Salmonella Rissen |
| Earliest known case onset date: 11/01/2008 | Latest case onset date: 05/27/2009 |
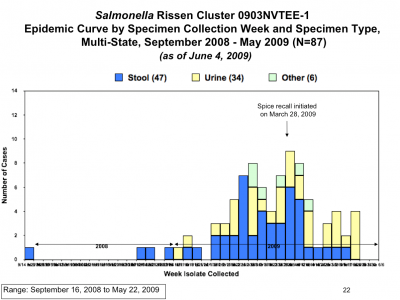
| Confirmed / Presumptive Case Counts: 87 / 0 | Positive Samples (Food): 33 |
| Hospitalizations: 8 | Deaths: 0 |
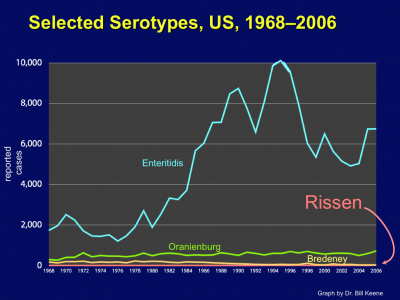
Salmonella Rissen is a very rare serotype in the US. When Oregon, California, and Nevada all reported it within days of each other, it began a coordinated investigation between those states (later to be joined by Washington and Idaho). This outbreak focused FDA attention on the role spices may play in salmonellosis outbreaks. Additionally, a large proportion of cases either had urine isolates or no gastrointestinal symptoms, making interviewing about food histories much more complicated.
Background:
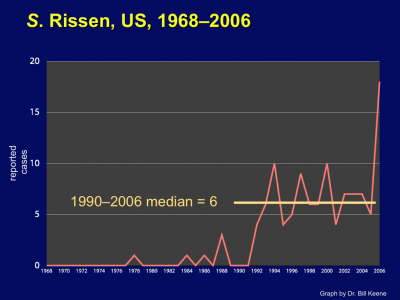
Salmonella Rissen is a very rare serotype in the U.S. with approximately 6 cases/year; in 2006 there was a sizable jump to 18 cases. Rissen is a fairly common serotype in Thailand, however; it is commonly associated with pork and chicken products.
On March 2, 2009, the Nevada State Public Health Laboratory posted a notification of a local cluster of Salmonella Rissen; CA and OR state health departments responded the same day to report similar local clusters—definitely above the expected annual baseline. In fact, this was the first reported outbreak of Salmonella Rissen in the United States. Washington and Idaho would later join the investigation with locally reported cases. CA and NV cases were clusters in the San Francisco Bay and Carson City/Reno areas, respectively.
Methods and Results:
By consensus, cases with an identifiable onset date were interviewed with shotgun questionnaires. CDC reported that the only PFGE match in the PulseNet database was an FDA report of an isolate from Vietnamese black peppercorns in 2006. Although the significance of this finding was uncertain, we were aware of it and added pepper-related questions in all interviews.
Oregon noted that they had one case who was Vietnamese and another who frequently ate at Vietnamese restaurants—fairly tenuous but about all we had to start with. An absence of travel histories implied a commercial product distributed primarily or exclusively in the West.
An extraordinary proportion of cases (63%) lacked what we could call a “clean” onset date—they either had vague symptoms going back for an indefinite period or had only urine isolates, sometimes with no referable GI symptoms.
Cases broke out into three distinct populations:
•Approximately half of the cases either had exposure to Asian restaurants or foods or had Asian surnames who cooked traditionally Asian foods at home (Generally younger and healthy)
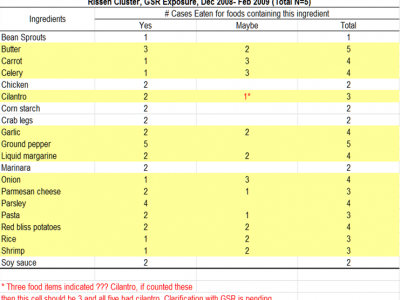
•Cases exposed to same large casino buffet in Nevada (exposures occurred between 12/08-2/09)
•35% of cases were hospitalized prior to or during time of specimen collection (generally older with underlying health conditions); they were at different facilities all under the same HMO organization.
At least 18 hypothesis-generating interviews were conducted using a hybrid of the Oregon shotgun and other more open-ended questions to explore longer time periods and more vague food exposures. Instead of using the standard time period of 7 days to go back and assess foods consumed prior to illness, we expanded the question over weeks and sometimes months of time; so many cases had little or no GI symptoms we wanted to cast a wide net when asking about exposures.
Nothing strongly suggestive emerged from those analyses other than the obvious clustering of NV and CA cases who had visited and eaten at Casino A in Reno. Efforts to identify common foods there foundered on the combination of poor recall and all-you-can-eat buffet overload. Some product testing was attempted, but initial results were all negative, including black pepper. NV initially suspected cilantro to be the culprit and were waiting to get confirmation that a buffet reservation had contained it at an ingredient; the decision was made not to test the black and white ground pepper that had been collected from the buffet in the first round of testing. All buffet ingredients that were initially tested came back negative.
(CONTINUED BELOW ↵)
• Bean sprouts: 33% cases vs. 12% FoodNet;
– OR 3.8, exact 95% CI 0.8-14.5, p=0.04
– Cumulative (binomial) probability = 0.0154
• Cilantro: 55% cases vs. 35% FoodNet;
– OR 2.3, exact 95% CI 0.6-9.5, p=0.20
– Cumulative (binomial) probability = .0597
• Black pepper: 67% cases, no FoodNet data available
Oregon decided to pursue brute force testing at two different restaurants frequented by one case (i.e., not really “implicated” in any way). This case had a urine isolate of Salmonella Rissen that was tested as follow up to a urinary tract infection and only reported one instance of loose stools (i.e., diarrhea); the case ate the named restaurant in the 3 days before illness. Food and spice samples were collected and split between IEH Laboratories in Seattle and the Oregon State Public Health Laboratory. Both labs isolated Salmonella Rissen from an open 5# container of Lian How brand white pepper collected at a Chinese/Vietnamese restaurant where the case added white pepper from a shaker into Pho (Vietnamese noodle soup). The Oregon PHL also recovered Rissen from a similar and adjacent container of black pepper. California Food and Drug Branch and the FDA worked with Union International Food Co. (Union City CA), which quickly led to a “voluntary” recall of Lian How and Uncle Chen brand pepper products on March 30, 2009—and soon expanded include everything that they packaged or prepared because of gross environmental contamination with Salmonella.
We worked with local and ODA environmental health staff to trace product distribution in Oregon and to reach out to restaurant operators who may have received the product. Language barriers and other considerations made us chary of relying solely on the media or the efforts of product distributors.
The final official tally was 87 cases in OR, WA, ID, NV, and CA; eight of the cases were Oregon residents. Clean onset dates occurred between 12/09/2008 and 04/29/2009 and could only be establish for 32 (37%) of cases. Rissen was isolated from stool specimen in 54% of the cases and from urine specimen in 39% of the cases. Ages ranged from 5 months to 94 years old with a median of 52 years old. Females accounted for 64% of the cases. Eight people were hospitalized due to GI illness (in all states).
Quantitative testing of three white pepper samples (recovered from 3 different Oregon restaurants) was performed by IEH Laboratories; results were 14 MPN/g, 2,400 MPN/g, and 14,900 MPN/g.
Conclusions
Contaminated white pepper was the cause of this outbreak. The positive black pepper sample was never replicated at any other lab and may have resulted from cross-contamination (most likely at the restaurant).
This outbreak (and the later Daniele salami outbreak) has focused FDA attention on the role spices may play in salmonellosis outbreaks; there are ongoing efforts in this arena.