| Outbreak: Polka Festival C. perfringens |
|---|
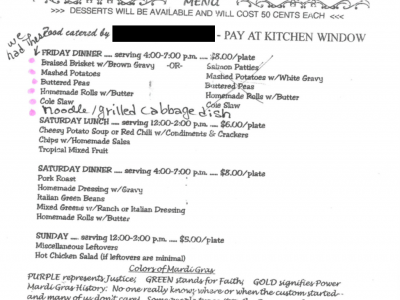
| Product: Catered dinner (mashed potatoes, beef brisket, gravy, rolls, and holuski) |
| Investigation Start Date: 3/14/2011 |
| Location: El Paso County, Colorado |
| Etiology: Clostridium perfringens |
| Earliest known case onset date: 3/11/2011 |
| Latest case onset date: 3/13/2011 |
| Confirmed / Presumptive Case Counts: 3 / 27 |
| Positive Samples (Environmental): N/A |
| Outbreak Summary: |
|---|
| A cluster of gastrointestinal illnesses due to Clostridium perfringens intoxication occurred following a catered dinner at a Polka Festival in El Paso County, Colorado on March 11-13, 2011. The caterer for this event was unlicensed, prepared all foods in their private home, and did not document food temperatures. |
| Details: |
|---|
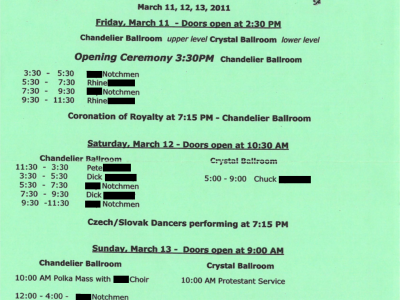
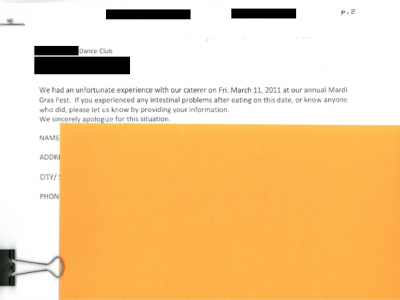
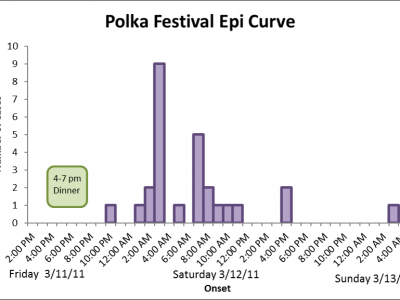
| Background On Monday, March 14, 2011, the Communicable Disease (CD) program at El Paso County Public Health (EPCPH) was contacted by a Dance Club regarding a cluster of gastrointestinal illness that occurred during a weekend Polka Festival. Approximately 120 persons participated in the festival, which began with a catered dinner and dance event starting at 4:00 pm on Friday, March 11. Initial reports indicated that 26 attendees had become ill with gastrointestinal symptoms in the early morning on March 12. Methods/Results A questionnaire was developed and included questions on symptoms, illness onset, and food and other exposures. Between March 15-17, the questionnaire was administered by phone to the cohort of festival attendees who were identified from an attendee list. A supplemental questionnaire was administered to food handlers for the event and contained more detailed questions about previous illness, hand hygiene, and food handling practices. Stool specimens were collected from ill persons and sent to the Colorado Department of Public Health and Environment (CDPHE) laboratory for norovirus PCR testing, sapovirus PCR testing, bacterial toxin testing, and routine bacterial culture. No leftover food items from the event were available for testing. A case was defined as a person having diarrhea (defined as three or more loose stools in a 24-hour period) after attending the Friday night event of the Polka Festival with onset of illness March 11-13. Based on the temporal clustering of illness onset, only interviewed persons who attended the Friday night event were included in the analysis. Ninety-two Polka Festival attendees were interviewed. Eleven attendees were excluded from analysis because they did not attend the implicated Friday night event; 81 attendees that participated in the Friday night event were included in cohort analysis. Twenty-seven persons met the case definition with a total attack rate of 33% for the dinner cohort. The ill persons ranged in age from 62-84 years old, with a median of 75 years old; 60% were male. Symptoms included diarrhea (1oo%), abdominal cramps (81%), nausea (33%), fever (7%), and blood in stool (4%). The three stool specimens collected from cases were tested at CDPHE and all three were positive for Clostridium perfringens toxin. The specimens were negative for all other testing. Food exposure analysis was done for all food items served at dinner on March 11 by the caterer, desserts sold at a bake sale, and beverages sold at a cash bar run by Dance Club volunteers. Exposure data collected from interviews were analyzed. Mashed potatoes, beef brisket, gravy, rolls, and holuski (a noodle and cabbage dish) all had elevated relative risk scores and were statistically significant. However, food exposure analysis was complicated by the fact that most people who ate the dinner had eaten some of each food item offered by the caterer. Environmental Health (EH) staff visited the owner of the catering company on March 14, 2011. This caterer did not have an active Retail Food Establishment (RFE) license when food for this event was prepared and had prepared food in their personal home rather than in a licensed commercial kitchen. The caterer indicated that all food, with the exception of the coleslaw, was prepared in their home the day before the event. Cooling of brisket, mashed potatoes, holuski and gravy was conducted in a home-style freezer and refrigerator at the caterer’s house. The size of food storage containers and time to cool the food to appropriate temperatures were not known and there was no documentation of food temperatures. EH staff were unable to observe food preparation techniques during the visit with the caterer. All food was transported in ice-cooled units in the caterer’s personal vehicle to the venue and temperatures were reportedly checked with a dial thermometer during transport. Transport took approximately 45 minutes. Brisket, mashed potatoes, gravy, peas, and holuski were removed from units and reheated to 160°F–180°F at the venue kitchen. Interviews with food handlers revealed discrepancies in the reported temperature to which food was re-heated. No temperature logs were kept. Food was served by food handlers employed by the caterer. Caterer stated that neither they nor their staff members were ill before or during the catering event. Environmental health staff also inspected the venue kitchen, where food was re-heated and served, on March 15, 2011. No critical violations were identified although the facility was not actively preparing food at the time of inspection. CD staff conducted interviews with nine persons who were either foodhandlers or served beverages at the dinner. No persons reported being ill with gastrointestinal symptoms during the two weeks prior to the event. Conclusions EPCPH CD and EH staff investigated a gastrointestinal outbreak at a weekend Polka Festival caused by bacterial intoxication from Clostridium perfringens. At least twenty-seven people met case definition with illness onset following a dinner and dance event on March 11. The epidemic curve was consistent with a point source as there was tight clustering of illness onset among people who ate the dinner meal on March 11. No other common exposures were identified among the Dance Club attendees other than the implicated dinner. The observed clinical illness showed a short incubation period, tight clustering of illness onset, relatively brief duration of diarrheal illness and lack of secondary cases, which are characteristic findings for C. perfringens intoxication. The environmental health investigation identified several potential risk factors with food preparation by the caterer that may have contributed to C. perfringens contamination, namely time and temperature abuse during storage, transport, and reheating of food. In this outbreak, five food items were statistically linked with illness: mashed potatoes, beef brisket, gravy, rolls, and holuski. Mashed potatoes, brisket, and gravy had the highest risk ratios. Historically, these foods have been commonly associated with outbreaks of bacterial intoxication. However, it is possible that the rolls and holuski were statistically significant because most people who ate any food from the caterer ate some of each food, making the implication of a single food item difficult. |