| Outbreak: Lighthouse Retreat Shigella |
|---|
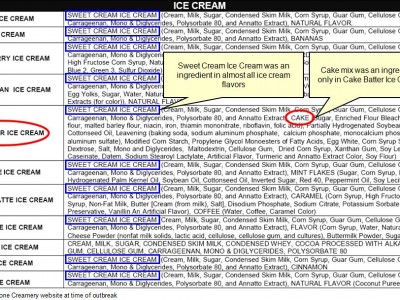
| Product: Never pinpointed |
| Investigation Start Date: 7/28/2005 |
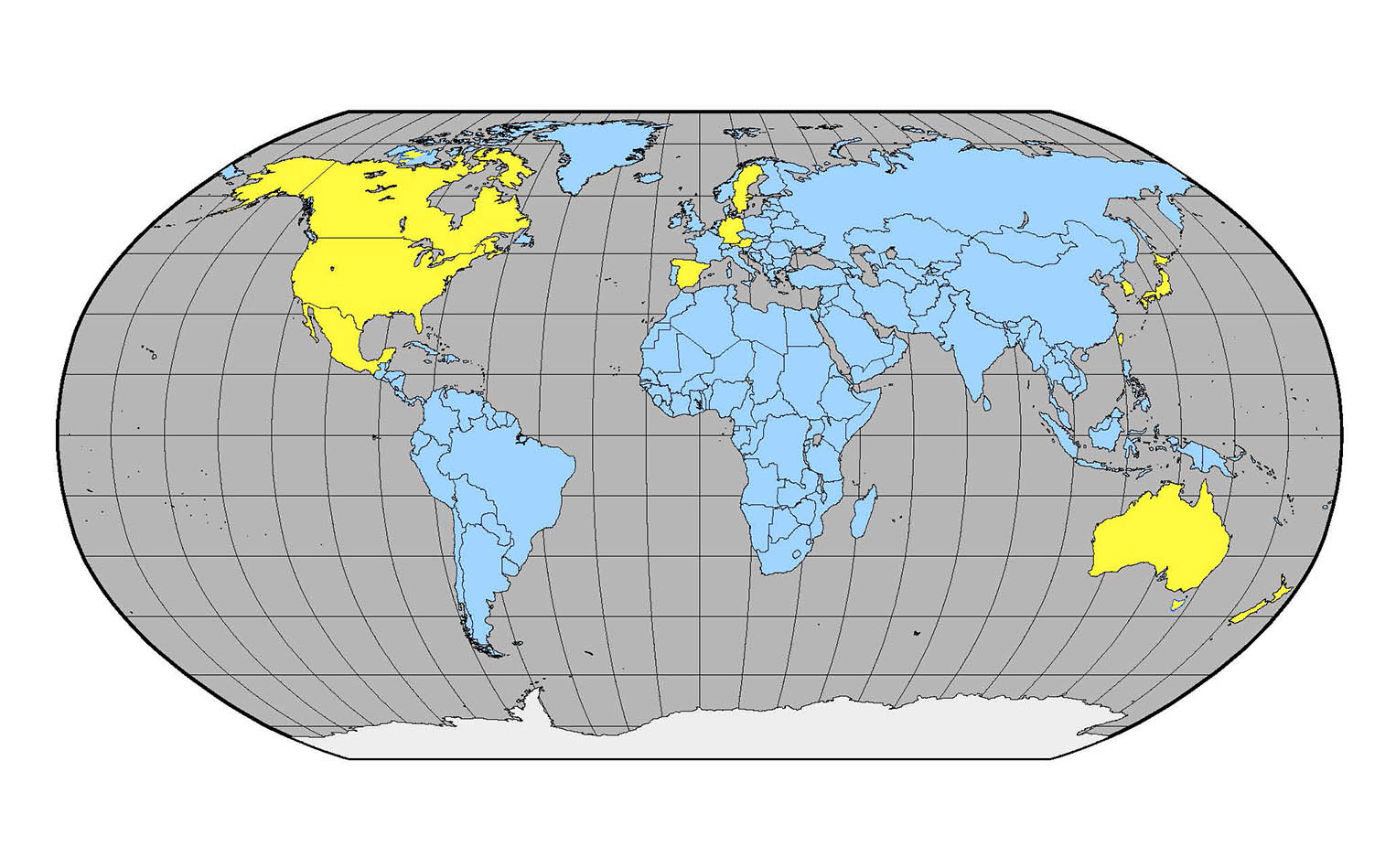
| Location: Douglas County, OR |
| Etiology: Shigella |
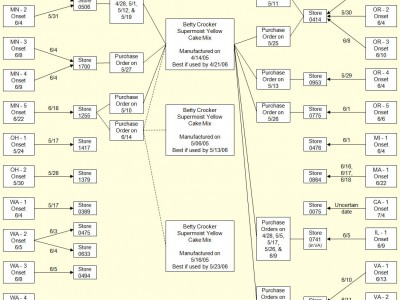
| Earliest known case onset date: 07/19/2005 |
| Latest case onset date: 08/06/2005 |
| Confirmed / Presumptive Case Counts: 18 / 262 |
| Positive Samples (Food / Environmental): 0 / 0 |
| Outbreak Summary: |
|---|
| This outbreak of shigellosis is one the largest Oregon has ever seen with at least 280 cases identified (18 of which were lab-confirmed). |
| Details: |
|---|
| A local organic farm and meditation retreat center hosted its annual 16-day retreat in 2005; the ill were among 1,400 people from 38 states and 21 foreign countries who converged on the center between July 22 and August 7. Daily attendance was ~750 people but this fluctuated with people coming and going. Most visitors had been staying for 1 to 4 weeks. The even was organized and executed by volunteers and 20 permanent staff members. Though this is a farm, no animals were kept on site. The group meals (only vegetarian) were prepared in one of two kitchens and consumed in a barn converted into a mess hall. Group meetings and meditation, as well as volunteer work, happened multiple times each day. Attendees camp or bunk on site and there were 55 portable toilets and sinks brought in for the event. We identified 280 persons who met the case definition for shigellosis; 250 saw a clinician and 9 were hospitalized. Many had come from around the world and made closing the camping areas seem like a poor option. Water samples were collected and did not yield positive results; food samples were not available for testing. The source of the outbreak was not found; it is likely that a human carrier working in the food prep or serving area contaminated some food items, which led to point source spikes in the epi curve (“simultaneous” infection, following one or two meals). Once Shigella seeded into this temporary community, it spread through a person-to-person route; difficult hygiene conditions at the center made this a plausible scenario. Putting disease control measures rapidly into place was critical for stopping the outbreak at this mass gathering event. |