| Outbreak: Jack In The Box Hamburgers |
|---|
| Product: Hamburgers |
| Investigation Start Date: 01/12/1993 |
| Location: Multi-State Outbreak |
| Etiology: E. coli O157 |
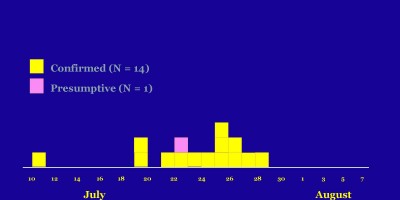
| Earliest known case onset date: 11/18/1992 |
| Latest case onset date: 02/21/1993 |
| Confirmed / Presumptive Case Counts: 503 / 229 |
| Positive Samples (Food / Environmental): 0 / 0 |
| Hospitalizations: 151 |
| Deaths: 3 |
| Outbreak Summary: |
|---|
This was the largest outbreak of E. coli O157 infections ever documented in the United States, and it injected this pathogen—and threats to food safety in general—into popular consciousness.
|
| Details: |
|---|
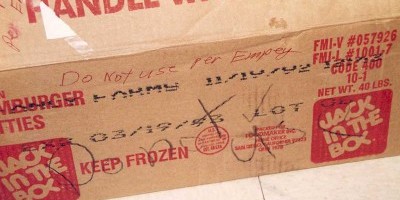
| On January 12, 1993, a pediatric gastroenterologist notified the Washington State Department of Health (WSDOH) of an increase in emergency department visits for bloody diarrhea and the hospitalization of three children with hemolytic uremic syndrome. Hypothesis-generating interviews suggested exposure at Jack In The Box restaurants, and in a swiftly conducted matched case-control study WSDOH confirmed association of illness with Jack-in-the-Box hamburgers. After news of the Seattle outbreak broke, clusters of bloody diarrhea and lab-confirmed E. coli O157 infections were soon recognized as associated with Jack In The Box hamburgers in California, Nevada and Idaho — an association confirmed by molecular testing by the newly developed Pulsed-Field Gel Electrophoresis (PFGE)method. Observation of cooking methods revealed that hamburgers did not consistently reach internal temperatures lethal for E. coli. Product trace-backs implicated selected lots of hamburgers (picture); culture of uncooked hamburger patties corroborated the epidemiologic findings. (1) Several pivotal public-health initiatives were undertaken in this outbreak's wake: 1. At the time of the outbreak, E. coli O157 infection was reportable in only 12 states. By the end of 1994, 33 states had made it reportable, and by the end of 1996, it was reportable in all but 6 states. 2. The outbreak "broke" the weekend of Bill Clinton's first Presidential inauguration, and it was one of the first exigencies that faced the new administration. Agriculture Secretary Mike Espy proposed sweeping changes to existing regulations regarding beef production, which had required only visual inspection of beef-processing operations. Under the new rules, USDA began testing samples of raw ground beef in 1994 for E. coli O157, which was declared an "adulterant," indicating a zero-tolerance policy for its presence even in uncooked beef; and in 1996 required the risk-reduction system known as "Hazard Analysis & Critical Control Points" (HACCP) in meat-processing establishments. 3. A renewed emphasis on foodborne illness was undertaken at CDC. In 1995, "FoodNet" was initiated to capture detailed data regarding foodborne illnesses systematically and to conduct special studies into their sources. Today, food safety has public health prominence as one of CDC's "Winnable Battles." 4. The Jack In The Box outbreak was the first major use of PFGE -- a new DNA typing technique that could explore relatedness of bacterial isolates. CDC trained and funded state health departments to test bacterial isolates routinely using this method and to report to a centralized system, where widespread but low-level outbreaks could be detected. Today, this "PulseNet" system can be credited with detecting a substantial fraction of recognized foodborne outbreaks. References: 1. Tuttle et al. "Lessons from a large outbreak of Escherichia coli O157:H7 infections: insights into the infectious dose and method of widespread contamination of hamburger patties." |